Surgery Shouldn’t Be a Gateway to Addiction
But outdated insurance policies are contributing to an ongoing opioid addiction crisis.
Every year, 1 out of every 10 people who are prescribed opioids to manage postsurgical pain become long-term opioid users - that’s about 4 million new Americans every year. Why? Because they’re given opioid (sometimes called “narcotic”) painkillers when other, non-opioid options exist. Unfortunately, most of the time, these options aren’t available to patients because they aren’t adequately paid for by insurance.
We're Asking for ONE thing:
Medicare covers specific, FDA-approved, non-opioid options to manage postsurgical pain. Many private health insurance companies don’t. That needs to change.
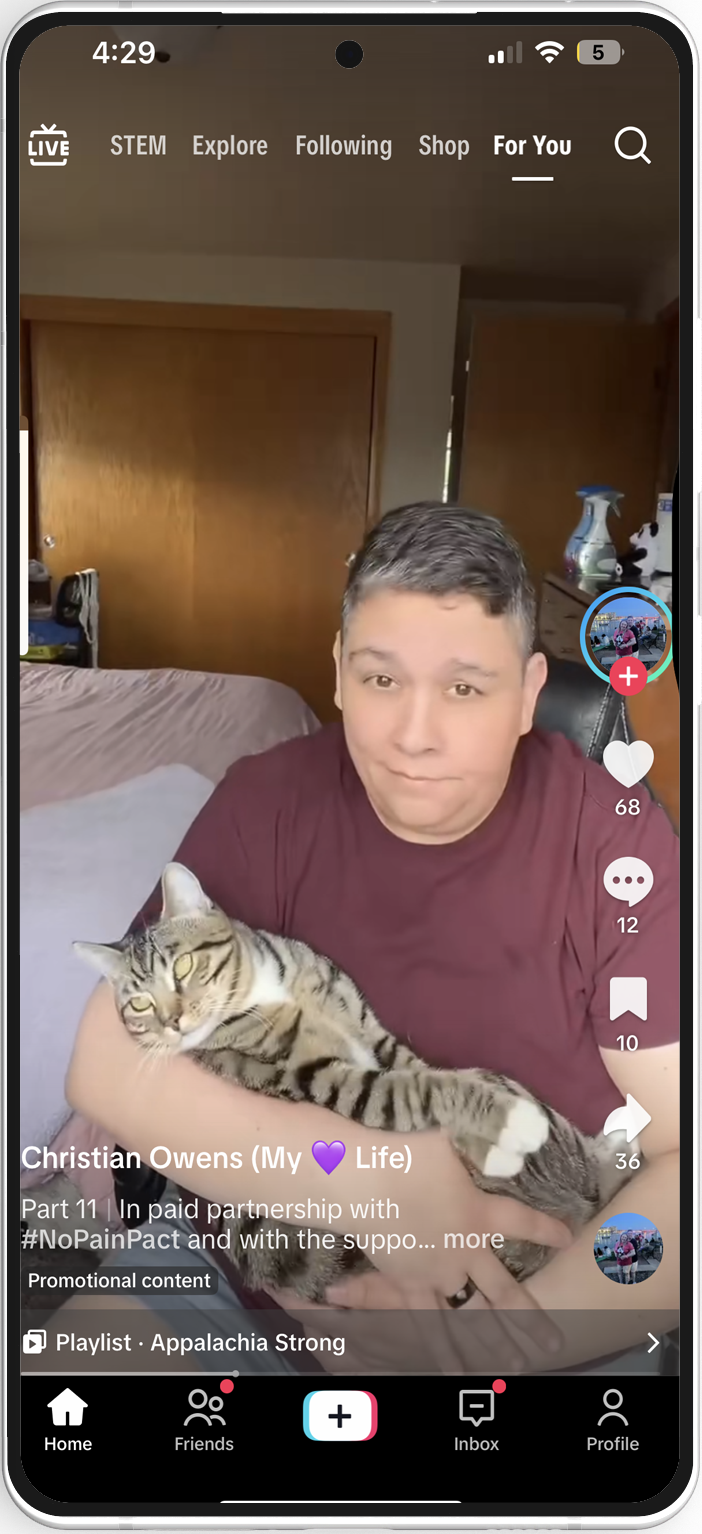
Join us! Share your story with a social post and ask:
“This is personal for me, but stories like mine are too common. What would your life look like if you or someone you love had never been exposed to opioids? Tell me in the comments and tag your health insurance company. They need to hear from you.”
#RethinkPainRelief #StopOpioidAddiction #NonOpioidsNow #HealthInsuranceFail
What Congress Did—and Private Health Insurance Companies Won't
In 2022, Congress passed the NOPAIN Act, a bipartisan law with a clear goal: to stop opioid addiction before it starts.
The law requires Medicare to fully cover qualifying non-opioid options used to manage postsurgical pain, like long-acting numbing agents and nerve blocks, nerve stimulators, and cryotherapy devices. These treatments help control pain without relying on opioids, lowering the risk of long-term use, addiction, and overdose.
Here’s what the NOPAIN Act changed:
Before the law
Facilities were discouraged from using non-opioid options because of short-term cost considerations because Medicare did not pay separately for them.
After the law
Medicare now pays separately for these non-opioid tools when used in outpatient surgeries. That means hospitals can offer these non-opioid options without being penalized financially.
Congress understood the need to prevent opioid addiction whenever we can. It’s a shame that too many health insurance companies refuse to make the same changes. And they won’t—unless we make them.
It’s a smart, simple fix. And it works. So, what’s the problem?
What Your Health Insurance Company Still Isn’t Doing
Despite all the evidence, and despite what Medicare now covers, many private insurance plans refuse to follow suit.
They Either:
Don’t cover these FDA-approved non-opioid tools at all, or
Only cover them in a bundled payment (vs. separately reimbursing for their use), which discourages hospitals from using them because they lose money when they do.
Every patient deserves the same options, not just those on Medicare. They should cover non-opioid options the right way: clearly, separately, and without barriers.
Because all patients deserve choices in how they manage their pain.
Health insurance company policies take that choice away from you. These same companies can do better, and doing better means making sure that patients can easily access a non-opioid pain management option if it makes sense for them.
Let’s work together with these companies to change the status quo. Stop defaulting to opioid-based pain protocols and put pain management decisions where they belong: in your hands.
#RethinkPainRelief
#StopOpioidAddiction
#NonOpioidsNow
#HealthInsuranceFail
©2025 Voices for Non-Opioid Choices,
750 9th Street N.W. – Suite 650 | Washington, DC 20001
A nonprofit 501(c)(4) organization.